Value Based Care - The Unique Connection
A for profit business is about that, making a profit. Fee for services is about the exchange of a service for payment. In a healthcare setting, the model contradicts terms of usage when the health care provider receives a payment for each service like an office visit, test, procedure, or other health care service. The cost of treatments are not of a concern, too much, because those costs are most likely covered by an insurance company. Many have perceived Fee for Service (FFS) as an obstacle to coordinating the patient pathway through the care continuum. It rewards individual clinicians for performing separate treatments, in a silo, if you will.
The advancements of technology have allowed a viewpoint into these specific nuances of care that offer the details needed to possibly circumvent a hospital stay, a call for an ambulance or another type of medical crisis help line. It's in these interoperable details that technology exhibits a dashboard to the provider to pay attention to even the most costly patients and managing the health outcomes with more scrutiny. These technological
opportunities open the doors to more effective business models and pricing that rewards the coordinated team for better patient outcomes rather than promote the incentive for services that add up the fees. The FFS payment model in healthcare will be a relic of the past and value-based care models may not be a final answer. The technology allows us to build and capitalize on a great system. With a well-educated and talented clinician base, the best medications, and science and research, the economics of the system should never waver or teeter on the edge of bankruptcy.
The pressure cooker is starting to steam. The Western world is aging and as society ages, so does the incidences of chronic disease and its care expense. We are aging and we are living longer. This comes with a price and that cost is appearing to be more unsustainable as we look into the future. The principles of value-based care (VBC) will address the high costs, and wastes of expenditures while focusing on what patients value and allocates resources according to the health outcomes delivered by the system.
Michael Porter, the business strategists and Professor at Harvard Business School, originally framed the outline for the value based care model. To simplify, VBC is to align processes and incentives. It begins by measuring outcomes for a particular patient, generate these outcomes to a population segment and then applying those insights to tailor and improve interventions across the care pathway for many similar patients. The bigger challenge is to allocate an objective payment that is weighted according to how well the system performed for the patient.
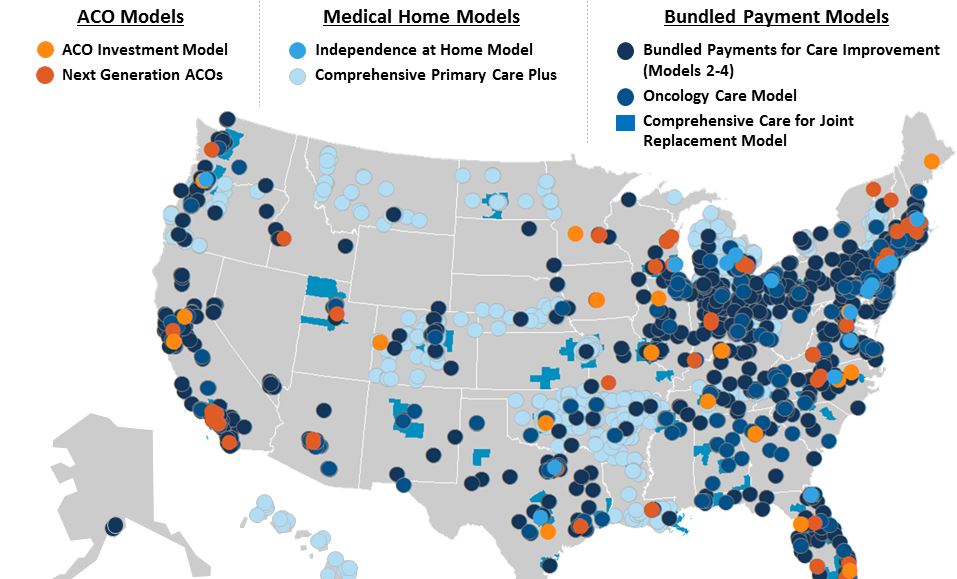
Optimism is the most important element of this model however. Without the fanfare, technology allows us to study, compare, measure, build and integrate sophisticated health informatics. We are exactly at the place we have been hoping to be. The ability to command powerful data analytics' networks into useful information that will improve science, patient lives and pricing. In its path have been iterative models to help develop skills and insights as with the development of the Accountable Care Organizations (ACOs), population health initiatives, patient engagement, clinical decision support, care coordination, and collaboration of the most unusual group to include quality metric specialists, pharmaceutical manufacturers, hospitals, and payers.
The advancements of technology have allowed a viewpoint into these specific nuances of care that offer the details needed to possibly circumvent a hospital stay, a call for an ambulance or another type of medical crisis help line. It's in these interoperable details that technology exhibits a dashboard to the provider to pay attention to even the most costly patients and managing the health outcomes with more scrutiny. These technological
opportunities open the doors to more effective business models and pricing that rewards the coordinated team for better patient outcomes rather than promote the incentive for services that add up the fees. The FFS payment model in healthcare will be a relic of the past and value-based care models may not be a final answer. The technology allows us to build and capitalize on a great system. With a well-educated and talented clinician base, the best medications, and science and research, the economics of the system should never waver or teeter on the edge of bankruptcy.
The pressure cooker is starting to steam. The Western world is aging and as society ages, so does the incidences of chronic disease and its care expense. We are aging and we are living longer. This comes with a price and that cost is appearing to be more unsustainable as we look into the future. The principles of value-based care (VBC) will address the high costs, and wastes of expenditures while focusing on what patients value and allocates resources according to the health outcomes delivered by the system.
Michael Porter, the business strategists and Professor at Harvard Business School, originally framed the outline for the value based care model. To simplify, VBC is to align processes and incentives. It begins by measuring outcomes for a particular patient, generate these outcomes to a population segment and then applying those insights to tailor and improve interventions across the care pathway for many similar patients. The bigger challenge is to allocate an objective payment that is weighted according to how well the system performed for the patient.
Optimism is the most important element of this model however. Without the fanfare, technology allows us to study, compare, measure, build and integrate sophisticated health informatics. We are exactly at the place we have been hoping to be. The ability to command powerful data analytics' networks into useful information that will improve science, patient lives and pricing. In its path have been iterative models to help develop skills and insights as with the development of the Accountable Care Organizations (ACOs), population health initiatives, patient engagement, clinical decision support, care coordination, and collaboration of the most unusual group to include quality metric specialists, pharmaceutical manufacturers, hospitals, and payers.
a few
VBC Models
|
Harnessing technology's strength is only as good as those who envision and act on its opportunity.
|
StrategyHarnessing technology's strength is only as good as those who envision and act on its opportunity.
Tactics: We envision a holistic, HIPAA compliant, 360-degree view of a patient population, or individual, used to research new advancements, reduce costs, and even cure or prevent the onset of diseases. Ultimately, this improves care personalization and efficiency while augmenting value-based models. We will do this by using trusted data resources and A.I. technology, which will make analysis faster and more accurate for our clients. Outcomes: A consortium of private-public opportunity available to tap a trusted, secure, and compliant resource with encrypted, skilled and talented resources, proprietary A.I. (Artificial Intelligence), data automation, cloud computing, data inspection and verification, reporting, analyses and decision-making tools. The application is intended for pharmaceutical companies and healthcare providers to improve patient outcomes and population health. |
|
Reached multiple stakeholders inside Integrative Delivery networks (IDNs) at the accounts that matter most for long-standing diabetes drug, with additional FDA-approved indications.
|
StrategyReached multiple and specific stakeholders inside Integrative Delivery Networks (IDNs) at the accounts that matter most for long-standing diabetes drug with additional FDA- approved indications.
Tactics: Built and managed target account list in a centralized location for campaigns. Reached target audiences with ‘zero waste’ advertising that attracted only the accounts targeted. Identified anonymous website visitors to know which accounts are coming to site (and which are not). Engaged each visitor with a website experience that delivered the right content at the right time. Outcomes: Program integrated account based marketing tools. Campaign engagement exceeded expectations at 35% CTR. |
|
This hospital enterprise was chosen as the US first round of ACOs continuing to build into value based care model today.
|
StrategyHospital system was always at the cutting edge and it continued in that spirit becoming of the first Accountable Care Organizations (ACO) in the country. Originally established in 2012, an ACO is a group of healthcare providers who voluntarily come together to coordinate healthcare services and engage in value-based payment models.
Tactics: With its inception, this hospital enterprise was chosen as the US first round of ACOs. It was developed into the Medicare Shared Savings Program (MSSP), a program developed by the Centers for Medicare and Medicaid Services (CMS) with the goal of encouraging providers to improve the quality of care provided to Medicare fee-for-service beneficiaries, while reducing the total costs of caring for such patients. Outcomes: The program’s evolution, from this inception yo present day, now participates in value-based models effectively and competitively to be the largest in its State. |
Business and Partnership Inquiry |
Social Media |
|